TMD is the second most popular musculoskeletal symptom in the US
By Namwook Cho L.Ac.
Jar-related pain patients are easily seen in an acupuncture clinic. The symptom is the second most popular musculoskeletal disease following chronic low back pain in the US.
Treatment of the symptom could be easy. The real problem is we do not have not much information in Western medical knowledge and language to diagnose and evaluate the symptom.
Clinical Practice Guideline of Korean Medicine for treating TMDs-related symptoms, published by the National Institute for Korean Medicine Development in Korea, provides the most valuable clinical information regarding Temporomandibular disorders (TMDs).
It showed scientifically proven treatment methods for acupuncture and herbal medicine. Also, tools for diagnosis and evaluation will be introduced.
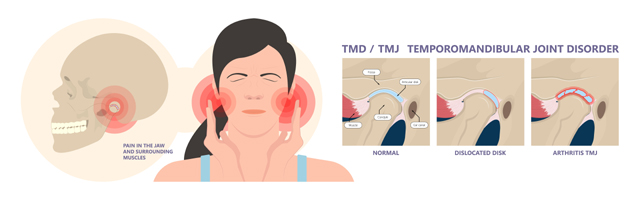
Definition: Temporomandibular disorders (TMDs) are “musculoskeletal and neuromuscular conditions occurring in the temporomandibular joint region, masticatory musculature, and associated structures.” TMDs consist of two main conditions: pain-related disorders (i.e., muscular pain, headache, and arthritic pain) and temporomandibular joint-associated disorders (i.e., articular disc disorder and degenerative joint disease).
Risk factors: Risk factors for TMD include sex (female), age (aged between 18 and 44 years), comorbidities (e.g., mood disorders and rheumatoid arthritis), behavioral factors (e.g., bruxism), pain hypersensitivity, and trauma. While the mechanism of TMD is not clearly understood, a combination of biological, behavioral, and environmental factors and perception changes are considered to contribute to its pathogenesis.
Diagnosis and tests: TMDs are diagnosed through evaluation of medical history and physical examination, and the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD), developed in 2014, is the widely accepted tool for diagnosis.
TMD Pain Screener is the most frequently used tool to diagnose and evaluate pain due to TMD. The test is composed of questions regarding the symptom. Each answer could be converted. An ‘a’ response is O points, a ‘b’ response is 1 point, and a ‘c’ response is 2 points. If the total converted answer reaches more than 3, it is diagnosed as pain-related TMD.
Treatment goal: In the hospital, non-pharmacologic and pharmacologic treatments are mostly used as conservative treatments for TMDs. Non-pharmacologic treatment commonly consists of patient education, self-care, behavioral therapy, occlusion stabilizers, and physiotherapy, while nonsteroidal anti-inflammatory drugs (NSAIDs), anti-depressants, and muscle relaxants are often prescribed as pharmacological treatment. Although surgery is also a treatment option, it should only be considered in patients who do not respond to non-surgical treatment over 3~6 months.
Treatment recommendation: Survey results on the clinical practice of KMDs’ treatment for TMD showed that acupuncture (including electroacupuncture), Chuna manual therapy, pharmacopuncture (including bee venom therapy), intra-oral balancing devices, and herbal medicine were the most frequently adopted Korean medicine treatments for TMDs and a combination of Korean medicine treatments are also employed.
- Acupuncture/ Alone treatment: A/High: Acupuncture significantly improved pain and function recovery compared to sham or no-intervention controls. Therefore, acupuncture treatment is recommended for the clinical practice of TMD patients.
- Clinical consideration: For acupoints for TMD treatment, Ha-gwan (ST7), Hyeop-geo (ST6), I-mun (TE21), and Ye-pung (TE17) may be considered with A-shi points according to patient symptoms. In addition, application of electroacupuncture and heat acupuncture may be considered based on patient clinical characteristics.
- Add-on treatment(B/Moderate): When acupuncture was performed concurrently with the usual conservative treatment, significant pain and function recovery improvement was confirmed in adult TMD patients.
- Herbal medicine/ Alone treatment(B/Moderate): Herbal medicine treatment significantly improved in adult TMD patients compared to the usual conservative treatment. Therefore, herbal medicine treatment should be considered in the clinical practice of TMD patients to improve symptoms.
- Clinical consideration: Ssang-hwa-tang, Gal-geun-tang, Jak-yak-gam-cho-tang , Bo-jung-ik-gi-tang, Man-geum-tang, and Gamisoyosan may be considered as herbal medicine for TMD treatment.
Following is the test questionnaire.
|
1. In the last 30 days, which of the following best describes any pain in your jaw or temple area on either side? a. No pain b. Pain comes and goes c. Pain is always present 2. In the last 30 days, have you had pain or stiffness in your jaw on awakening? a. No b. Yes 3. In the last 30 days, did the following activities change any pain (that is, make it better or make it worse) in your jaw or temple area on either side? A. Chewing hard or tough food. a. No b. Yes B. Opening your mouth or moving your jaw forward or to the side. a. No b. Yes C. Jaw habits such as holding teeth together, clenching/grinding, or chewing gum. a. No b. Yes D. Other jaw activities such as talking, kissing, or yawning. a. No b. Yes |