- Manyong Park1,2 and Sungchul Kim1,2
1Wonkwang University Korean Medical Hospital, Department of Acupuncture & Moxibustion, Gwangju, Republic of Korea
2ALS Center ofWonkwang University Korean Medical Hospital, Gwangju, Republic of Korea - Hindawi Publishing Corporation, Evidence-Based Complementary and Alternative Medicine, Volume 2015, Article ID 703439, 8 pages
1. Introduction
Saam acupuncture, which is one of the original therapeutic modalities representing traditional Korean medicine, is a unique treatment method that has a different origin than the modalities from China and Japan. The basic characteristic of combining five shu points in Saam acupuncture is the selection of the tonification and sedation points along the self-meridian and other meridians based on creation and governor relationships. In China, five element acupuncture, tonification, and sedation points along only the self-meridian are selected. Japanese meridian therapy added source point, connecting point, cleft point, alarm point, and transport point on the basis of Korea Saam acupuncture conception of the combined five shu points [1].
Saam acupuncture is based on the traditional concepts of yin-yang, five elements, ZangFu (viscera and bowels), qi, and meridians. Saam acupuncture treatment cannot be separated from these viewpoints. In particular, it involves the application of five shu points according to the creation and control cycles of the five-element theory. Therefore, the combination of acupoints in Saam is easier to understand from the perspective of traditional medicine.
The meridian is divided into three parts: the arm or foot, three yin and yang, and six ZangFu parts. A total of 24 deficiency and excess symptoms, with 24 coldness and fire symptoms, exist across the 12 meridians, but the diagnostic criteria related to these symptoms are too ambiguous for selecting a correct meridian. Except for the regular 48-treatment protocol, the treatment strategies are largely variable. Efforts were made to produce Saam treatments that are more effective by including other acupoints, with the main points firmly based on the regular pattern [2].
However, because the explanation regarding acupoint selection is very brief or elided, applying Saam acupuncture in the clinic is difficult. Various Korean scholars have suggested different methods for applying Saam acupuncture in the clinic. Lee [3] proposed a diagnostic system by comparing pulse examination, whereas Kim [4] proposed a symptom-based diagnosis.
Cho [5] established visceral pattern identification for providing easy access to Saam acupuncture by analyzing Neijing (Internal Classic), Nan-jing (Classic of Difficult Issues), and Yixuerumen (Introduction to Medicine).Moreover, Kwon [6] studied constitutional acupuncture, and Kim[7] reviewed the mind-based aspect of Saam acupuncture.
However, a description of the mechanism of acupuncture to both clinicians and patients in mainstream medicine by using the contemporary concepts of neurobiology would be helpful for incorporating Saamacupuncture into mainstream medicine [8]. An important difference between traditional Korean medicine and the Western medical approach is the diagnostic process. In traditional Korean medicine, the diagnosis is made by using the principles of syndrome differentiation, which could be in accordance with the state of the ZangFu or qi or with the doctrine of the meridians [9]. This diagnostic process does not match the patterns in Western medicine.
In this paper, several neurobiological mechanisms of Saam acupuncture treatment are presented from the perspective of the clinician. Saam acupuncture clinical trials are also discussed. Further, the historical background of Saam acupuncture and the basic principle of combining acupoints are briefly reviewed.
2. The Historical Background of Saam Acupuncture
The original manuscript that described Saam acupuncture is estimated to have been published between 1644 and 1742, in the middle of the Cho Sun dynasty, by a Korean Buddhist monk whose name is unknown. Because Chimgoogyeongheombang (Experiential Prescriptions of Acupuncture and Moxibustion), which was published in 1644, is quoted in the manuscript of Saam acupuncture, the publication period of the Saam acupuncture manuscript can be estimated to be after 1644 [10]. After 1742, Gy-san’s clinical experience was added to the original manuscript of Saam acupuncture, that is, Gyeongjeyogyeol (Essential Rhymes on Acupuncture and Moxibustion by Master Saam). This is the oldest existing manuscript associated with Saam acupuncture. The physiology, pathology, and disease identification sections of Saam were handed down to its disciples, but the clinical experience section of Gy-san coexists in the currently published Saam acupuncture-related books [11].
Viscera/bowel-based acupuncture was developed in Chimgoogyeong-heombang (Experiential Prescriptions of Acupuncture and Moxibustion), with integration of the meridian/exterior theory with the viscera manifestation theory, which in turn provided various methods for viscera diagnosis. Viscera identification became the basis of Saam acupuncture treatment [12].
The Dongeuibogam (Treasured Mirror of Eastern Medicine) contains the following phrase: “One acupuncture needle in all the diseases, up to within four acupuncture needles, acupuncture on the whole body is not a good idea.”
This phrase represents the characteristics of the traditional Korean acupuncture method. In this context, Saam acupuncture treated the disease within four acupuncture points. Further, an acupuncture method based on the five element principles is presented in the acupuncture section of the Dongeuibogam. The idea of treating a disease derived from viscera/bowel dysfunction by using five shu points influenced Saam acupuncture [1].
3. The Basic Theory of Combining Five Shu Points in Saam Acupuncture
The following phrase is taken from the 69th chapter of Nanjing: “In the case of depletion, fill the respective mother, in the case of repletion, drain the respective child, one must fill the first and then drain afterward.” Gao-Wu, of the Ming Dynasty of China (1519 A.D.), was the first acupuncturist to describe the use of tonification and sedation points along the self-meridian by using the five shu points according to the 69th issue of Nan-Jing. Zhang Shi Xian advocated the use of five shu points in other meridians in Jiao Zheng Tu Zhu Nan Jing (Illustrated note of Classic of Difficult Issues) [11]. On the basis of Gao-Wu and Zhang Shi Xian treatment, Saam added the role of the governor. This notion originated from the 50th and 75th chapters of Nan-Jing.
In Saam acupuncture, the relationship with the governor is important, as is the relationship between the mother and son. The governor is sedated under the condition of deficiency and is tonified under the condition of excess [13].
The basic rules are those of the creation and governor relationships. In the case of insufficiency of any meridian, the mother points of its mother and its own meridians should be tonified and the governor points of its governor and its own meridians should be sedated. For example, the following is applied if the lung meridian is diagnosed as deficient: earth tonification, lung meridian-earth point LU9 and spleen meridian-earth point SP3 and fire sedation, lung meridian fire point LU10, and heart meridian-fire point HT8 (Table 1).
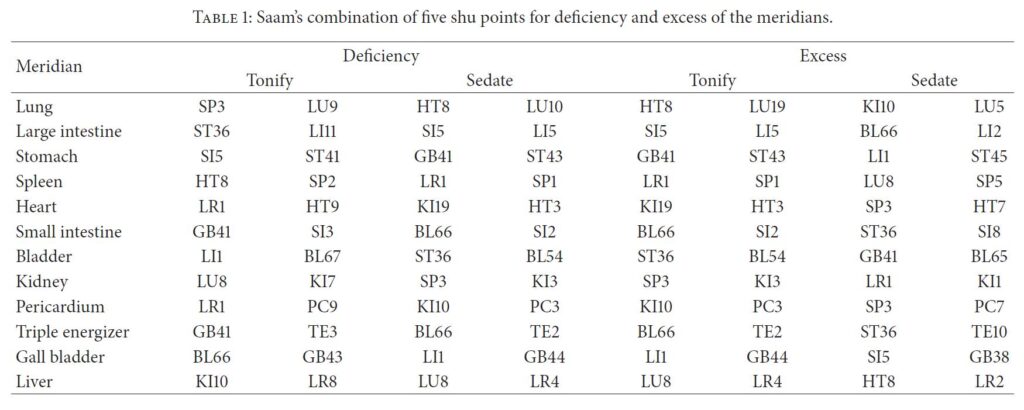
The other meridians follow the same rule, as described above. In the case of the excess of any meridians, the governor points of its governor and its own meridians should be tonified and the son points of its son and its own meridians should be sedated. For example, the following is applied if the lung meridian is diagnosed to be excessive: fire tonification, lung meridian-fire point LU10, and heart meridian-fire point HT8 and water sedation, lung meridian-water point LU5, and kidney meridian-water point KI10 (Table 2).
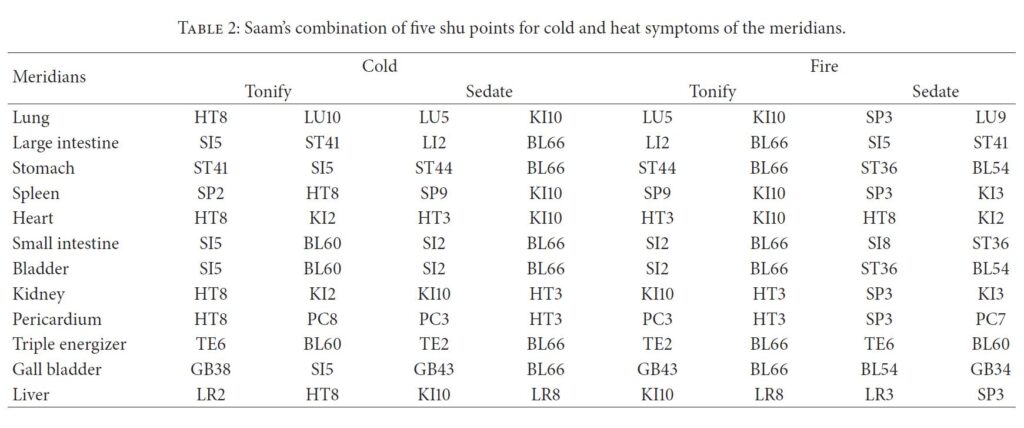 Another simple but rarely used one is coldness-fire acupuncture treatment derived from the deficiency-excess acupuncture treatment. For cold symptoms, the fire points of its own and the fire meridians are tonified and the Water points of its own and the water meridians are sedated. For heat symptoms, the water points of its own and the water meridians are tonified and the fire points of its own and the fire meridians are sedated (Table 2).
Another simple but rarely used one is coldness-fire acupuncture treatment derived from the deficiency-excess acupuncture treatment. For cold symptoms, the fire points of its own and the fire meridians are tonified and the Water points of its own and the water meridians are sedated. For heat symptoms, the water points of its own and the water meridians are tonified and the fire points of its own and the fire meridians are sedated (Table 2).
Among the clinical case studies of Saam, 85% used either a tonification or a sedation formula, whereas 15% used variations of the tonification and the sedation formulae [13]. Saam treatment primarily focuses on the viewpoints of deficiency-excess symptoms rather than cold-heat symptoms [1]. The 240 acupuncture treatments described in the Gyeongjeyogyeol consist of 100 regular forms on the basis of the 69th issue of Nan-Jing, 140 irregular forms on the basis of the 73rd and 75th issues, and various special acupuncture points, which include the source, connecting, accumulation, alarm, and back-transporting points [14].
References
[1] Y. O. Jung, D. H. Lee, and S.W. Ahn, “A research for tradition and identity of Saam acupuncture method,” Korean Journal of
Acupuncture, vol. 29, no. 4, pp. 537–553, 2012.
[2] C.-B. Ahn, K.-J. Jang, H.-M. Yoon et al., “A study of the Sa-Ahm Five Element acupuncture theory,” Journal of Acupuncture and Meridian Studies, vol. 2, no. 4, pp. 309–320, 2009.
[3] J. W. Lee,The Secret of Sa-Ahm’s Acupuncture Based on Yinyang and Five Elements, vol. 1, Institute for Studying Five Element Acupuncture, Busan, Republic of Korea, 1958.
[4] D. P. Kim, “Sa-Ahm’s five element acupuncture and its usages,” the Journals of the Korean OrientalMedical Society, pp. 122–123, 1972.
[5] S. H. Cho, The Systematic Research of Saam Acupuncture, Seongbo, 2001.
[6] D. W. Kwon, “Constitutional acupuncture,” The International Journal of Acupuncture and Moxibustion, pp. 149–167, 1965.
[7] H. K. Kim, Revolutionary Review of OrientalMedicine, Sinlong-Bonche, Seoul, Republic of Korea, 2001.
[8] K. J. Cheng, “Neurobiological mechanisms of acupuncture for some common illnesses: a clinician’s perspective,” Journal of
Acupuncture and Meridian Studies, vol. 7, no. 3, pp. 105–114, 2014.
[9] X. Cheng, Chinese Acupuncture and Moxibustion, Foreign Languages Press, Beijing, China, 1999.
[10] D. H. Kim, “The literary study on the written date and the background of Sa-Ahm’s 5 element acupuncture method,”
Journal of Korean Medical Classics, vol. 7, pp. 113–160, 1993.
[11] S. C. Kim, J. H. Won, and K. W. Kim, Korea Traditional Sa-Am Acupuncture, Jimoondang, 2009.
[12] J. Oh andN. Ki, “A study on the acupuncturemethods of Joseon Dynasty using five viscera diagnosis,”KoreanJournal of Oriental Medicine, vol. 16, no. 4, pp. 1–31, 2010.
[13] R. Cha, D. Yoon, J. Kim, M. Lee, and G. Lee, “A study of Sa-Ahm’s thoughts on the four-needle acupuncture technique with the five-element theory,” Journal of Acupuncture and Meridian Studies, vol. 7, no. 5, pp. 265–273, 2014.
[14] A. Hicks, J. Hicks, and P. Mole, Five Element Constitutional Acupuncture, Churchill Livingstone, Edinburgh, UK, 2005.