- Mikyung Kim(1Department of Internal Medicine, College of Korean Medicine, Sangji University), Chang-ho Han(Department of Internal Medicine, College of Korean Medicine, Dongguk University)
- J Korean Med. 2021;42(4):75-101
Study selection
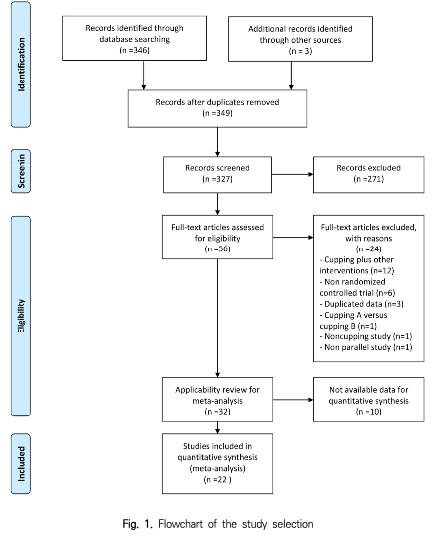
A total of 374 articles were identified through the database search, and 3 articles were identified through hand searching, and of these, 50 were excluded due to duplication.
The titles and abstracts of the remaining 327 articles were screened, and 271 articles not suitable for this study were excluded. Full texts of the remaining 56 articles were read and 24 articles that did not meet the eligibility criteria of this study were excluded.
Out of the remaining 32 articles, 22 articles providing data suitable for quantitative synthesis were finally selected for meta-analysis and methodological quality assessment.
The study selection process is summarized in Fig. 1, and a list of articles excluded during the process from full text reading to the final selection is presented in Supplement 4.
1. Characteristics of the included studies
1) Study design and sample size
A total of 22 studies11-32) with 1653 participants published in China from 2001 to 2020 were included in the final analysis. Most of them were studies with a 2-arm design with the exception of three studies14,19,31) with 3 arms. The number of participants included in the posttreatment evaluation ranged from 40 to 135 (Table 1).
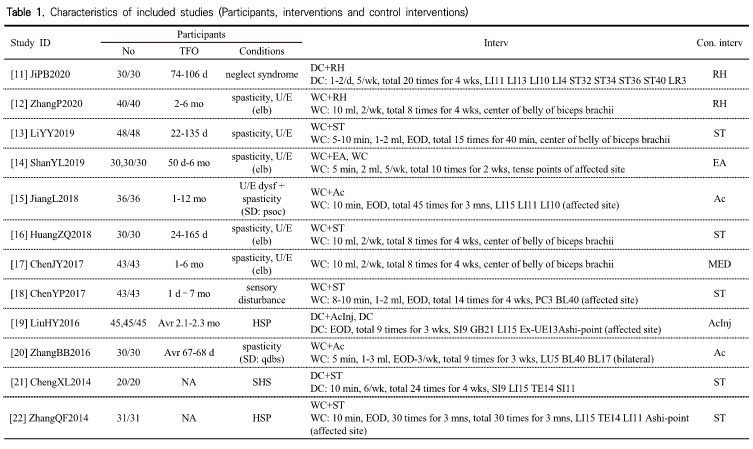
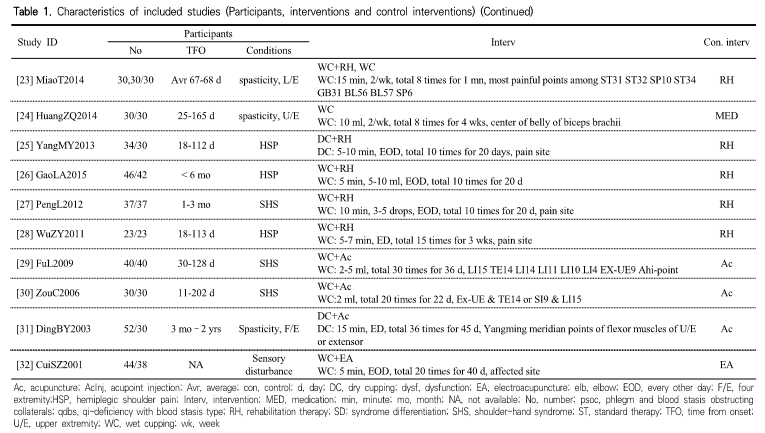
2) Participants
The participants of all included studies were patients with stroke, and none of the studies limited the stroke subtype of the patients. There was no study that recruited only patients in the acute stage within one week of stroke onset, but most of the participants were patients within 6 months of stroke onset. Of the exceptions, 4 studies included patients with more than 6 months since stroke onset,15,18,30,31) and 3 studies did not provide any information regarding the time from onset (Table 1)22,23,32).
The most commonly treated stroke condition was spasticity, which was reported in 9 studies 12-14,16,17,20,23,24,31). Six12-14,16,17,24) of these studies targeted patients with upper limb spasticity, of which 412,14,16,17) were about elbow spasticity.
There were three studies each on spasticity in lower limbs23), four limbs,31) and nonspecified parts20). The most commonly studied stroke conditions after spasticity were hemiplegic shoulder pain (5 studies)19,22,25,26,28) and poststroke shoulder-hand syndrome (4 studies).21,27,29,30) The remaining studies targeted sensory dysfunction18,32), upper limb dysfunction15), and neglect syndrome (Table 1)11).
Two studies considered the type of syndrome differentiation based on traditional Chinese medicine.15,20) One enrolled patients with spasticity and qi deficiency with blood stasis type15) and the other enrolled patients with upper limb dysfunction
with phlegm and blood stasis obstructing collaterals type (Table 1)20).
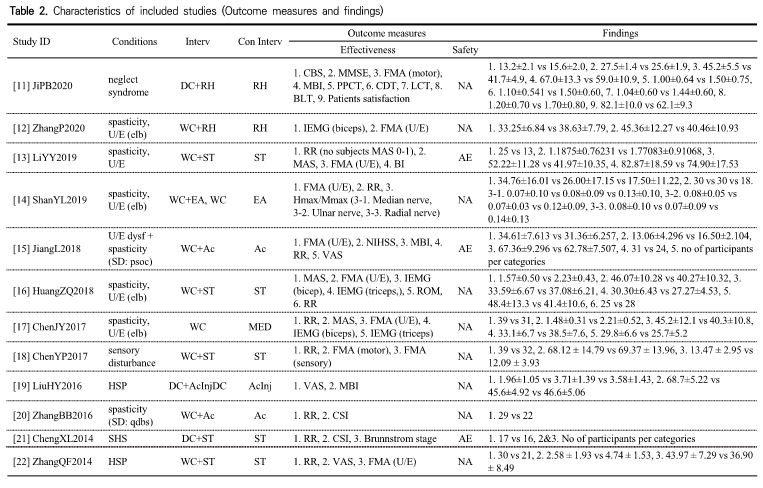
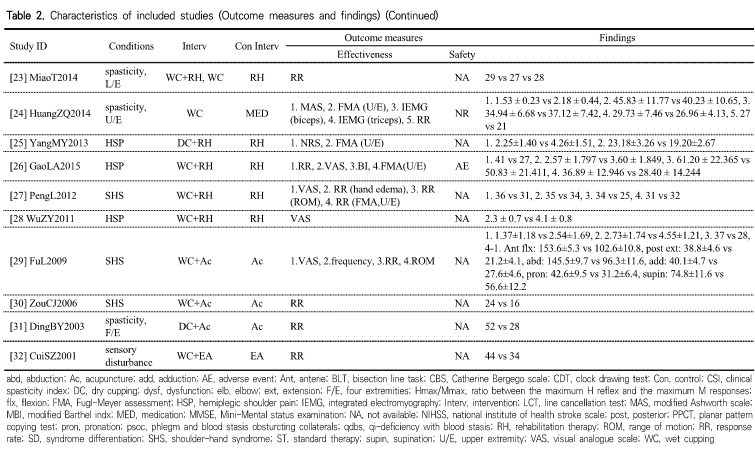
3) Intervention, control and outcome measures
- A versus B type studies
Two studies17,24) compared the effects of wet cupping and Western medication (baclofen, a muscle relaxant) in patients with upper limb spasticity. In both studies, the treatment period was 4 weeks, the treatment group received wet cupping on the center of the biceps brachii belly twice a week, and the control group was orally administered 10 mg of baclofen three times a day.
These two studies evaluated changes in upper limb motor function and spasticity. In terms of the safety of the cupping therapy, one study24) described the plan for adverse event monitoring in the methods session but did not report the results. Another study17) did not provide any information on the safety of cupping therapy (Table 1 & 2). - A+B versus B type studies
Twenty studies11-16,18-23,25-32) were designed as an A+B versus B form, comparing the add-on effect of cupping therapy with the noncupping control in patients receiving standard treatment for stroke. Three of them14,19,23) were 3-arm studies, and the other 18 were 2-arm studies. No studies used sham devices or placebo controls (Table 1).
Of the 20 studies, 511,19,21,25,31) used dry cupping and 1512-16,18,20,22,23,26-30,32) used wet cupping. The retention time for cupping was between 5 and 15 minutes in both dry and wet cupping studies. The amount of blood drawn by wet cupping therapy ranged from a few drops to 10 ml. Ten13,15,18-20,22, 25-27,32) of the included studies performed cupping therapy once every other day. The next most common protocols were once a day14,28,30,31) and twice a week12,16,23). The treatment period was most frequently 4 weeks11,12,16,18,21) and ranged between at least 2 weeks and at most 6 months.
The most common sites for cupping were the pain site of the affected shoulder for patients with hemiplegic shoulder pain or shoulder-hand syndrome and the center of the biceps brachii belly for patients with upper limb spasticity (Table 1).
The therapeutic effects of cupping therapy for stroke patients was evaluated on various scales. Most of the studies presented the response rates for the main outcomes in stroke survivors. In addition, many other studies measured upper limb motor function using the Fugl-Meyer assessment (FMA) scale, and there were also studies that evaluated overall motor function or sensory function. Some studies assessed the intensity of shoulder pain using a visual analog scale (VAS) or numeric rating scale. There were also studies that assessed the activities of daily living using the Barthel or modified Barthel index. There was only one study15) that assessed neurological deficits using an internationally accepted stroke scale, such as the National Institute Health stroke scale, and no study reported mortality, disability, or recurrence of stroke (Table 1 & 2).
Most studies did not mention safety. One study on dry cupping21) reported that any serious adverse events were observed, and three studies on wet cupping13,15,25) described the adverse events identified during the study period (Table 1 & 2).
References
- 10. Guyatt, G. H., Oxman, A. D., Schünemann, H. J., Tugwell, P., & Knottnerus, A. (2011). GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. Journal of Clinicial Epidemiology, 64(4), 380-382. doi: 10.1016/j.jclinepi.2010.09.011.
- 11. Ji, P. B., Wu, Z. Q., Jia, D. P., Wang, L., & Shu, Y. Y. (2020). Clinical Study of Colored Silica Gel Can Combined with Exercise Therapy for Unilateral Neglect After Stroke. Shanghai Journal of Acupuncture and Moxibustion, 39(8), 983-987. doi: 10.13460/ j.issn.1005-0957.2020.08.0983
- 12. Zhang, P., Chen, Y., Dai, W., & Nie, L. (2020). Observation on the effect of puncturing and cupping combined with rehabilitation training in the treatment of stroke patients with upper limb elbow flexion spasm and analysis of the effect of biceps integrated electromyography. China Rural Health, 12(20), 75.
- 13. Li, Y. (2019). Clinical Study of Blood – letting Puncture and Cupping Combined with Bobath Technique in the Treatment of Upper Limb Spasticity after Stroke. Chinese Journal of Ethnomedicine and Ethnopharmacy, 28(21), 84-86.
- 14. Shan, Y., Liu, J., Sun, L., Li, Q., & Wang, J. (2019). Therapeutic Observation of Collateral -pricking Cupping for Upper-limb Spasm in Patients with Cerebral Stroke. Shanghai Journal of Acupuncture and Moxibustion, 38(3), 270-274. doi: 10.13460/j.issn.1005-0957. 2019.03.0270.
- 15. Jiang, L. (2018). The Curative Effect of Acupuncture and Cupping Therapy on Upper Limb Dysfunction of Stroke Xinjiang Medical University [Master’s thesis].
- 16. Huang, Z., Zhao, N., Su, Z., Su, J., & Wu, Q. (2018). Effects of pricking and cupping combined with rehabilitation training on elbow flexion spasticity of upper limb after stroke and its IEMG value. Chinese Acupuncture & Moxibustion, 38(2), 119-124. doi: 10.13703/j.0255-2930.2018.02.002.
- 17. Chen, J., Lin, S. (2017). The clinical effect of pricking and cupping combined with rehabilitation training in the treatment of stroke patients with upper limb elbow flexion spasm. Chinese Journal of Medical Device, 30(15), 121-122.
- 18. Chen, Y. P. (2017). Clinical Research on Hemidysesthesia After Stroke Treated by Acupuncture combined with Collateral-Needling Cupping. Henan Traditional Chinese Medicine, 37(1), 87-89. doi: 10.16367/j.issn.1003-5028. 2017.01.0029.
- 19. Liu, H., Liu, T., & Wang, Z. (2016). Effect of acupoint injection combined with cupping treatment on the daily life ability of patients with shoulder pain after stroke. Chinese Community Doctors, 32(27), 169-170. doi: 10.3969/j.issn.1007-614x.2016.27.108.
- 20. Zhang, B. (2016). The Clinical Observation of Body Spasm After Stroke Applying The Therapy of Combination Acupucture With Pricking and Cupping. Shandong University of Traditional Chinese Medicine [Master’s thesis].
- 21. Cheng, X., Cheng, C. (2014). Cupping combined Conventional Symptomatic Treatment and Rehabilitation Training after Stroke Shoulder – hand Syndrome Randomized Parallel Group Study. Journal of Practical Traditional Chinese Internal Medicine, 28(11), 27-29. doi: 10.13729/j.issn.1671-7813.2014.11.12.
- 22. Zhang, Q., Wei, Z., Cui, Y. (2014), Bloodletting and cupping combined with exercise therapy to treat 31 cases of stroke and hemiplegia and shoulder pain.. Hebei Journal of Traditional Chinese Medicine, 36(4), 568-569.
- 23. Miao, T. (2014). MOTOmed intelligent exercise system combined with blood pricking and cupping for treatment of increased muscle tone of lower limbs in stroke patients. Practical Journal of Medicine and Pharmacy, 31(3), 214-215. doi: 10.14172/j.cnki.issn1671 -4008.2014.03.007.
- 24. Huang, Z. (2014). Effect of Pricking Blood with Cupping Therapy Combined with Rehabilitation Training on the Spasticity of the Upper Limb in Patients with Stroke. Fujian University of Traditional Chinese Medicine [Master’s thesis].
- 25. Yang, M. (2013). Rehabilitation training combined with cupping to treat 64 cases of shoulder pain after stroke. Forum on Traditional Chinese Medicine, 28(6), 26-27.
- 26. Gao, L., Chu, J., & Bao, Y. (2012). Observation on the effect of blood puncturing and cupping combined with rehabilitation on hemiplegic shoulder pain and upper limb motor function improvement after stroke. Zhejiang Journal of Traditional Chinese Medicine, 47(11), 821-823.
- 27. Peng, L., Wang, Z., Li, L. (2012). Research of Shoulder Hand Syndrome After Stroke Treated by Collateral Disease Theory. Journal of Emergency in Traditional Chinese Medicine, 21(3), 448-449.
- 28. Wu, Z., & Huang, W. (2011). Observation of puncture and cupping combined with rehabilitation training in the treatment of apoplexy and shoulder pain. Journal of Zhejiang Chinese Medical University, 35(3), 425. doi: 10.16466/j.issn1005-5509.2011.03.013.
- 29. Fu, L., Liu, W., Wu, Q., Li, X., Li, D., & Shi, X., et al. (2009). Observations on the Efficacy of Acupuncture Plus Pricking-cupping Bloodletting in Treating Postapoplectic Shoulder-hand Syndrome. Shanghai Journal of Acupuncture and moxibustion, 28(3), 132-134. doi: 10.13460/j.issn.1005-0957.2009. 03.003.
- 30. Zou, C., Zhu, G., & Bao, Y. (2006). Treatment of 30 Cases of Shoulder-Hand Syndrome after Apoplexy with Acupuncture and Collateral Puncture Cupping. Zhejiang Journal of Traditional Chinese Medicine, 41(6), 340.
- 31. Ding, B., & Cui, Y. (2003). Treatment of Hemiplegia and Joint Contracture after Apoplexy by Acupuncture plus Cupping
Therapy: A Report of 52 Cases. Journal of Acupucture and Tuina Science, 1(5), 38-39. doi: 10.1007/BF02874843. - 32. Cui, S. (2001). Observation on the Curative Effect of Plum-blossom Needle and Cupping in Treating Sequelae. Journal of External Therapy of Traditional Chinese Medicine, 10(4), 37.