Boram Lee1, O.-Jin Kwon1, Joo-Hee Kim2,3, Jung Won Kang4, Tae-Hun Kim5, Seunghoon Lee4, Jungeun Kim6, Ae-Ran Kim7, So Young Jung7, Hyo-Ju Park7 and Sun-Mi Choi 8,9 (Hindawi Evidence-Based Complementary and Alternative Medicine Volume 2022, Article ID 2581041, 11 pages
- 1 KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 2 Department of Acupuncture and Moxibustion Medicine, College of Korean Medicine, Sangji University, Wonju, Gangwon-do, Republic of Korea
- 3 Research Institute of Korean Medicine, Sangji University, Gangwon-do, Republic of Korea
- 4 Department of Acupuncture and Moxibustion, College of Korean Medicine, Kyung Hee University, Seoul, Republic of Korea
- 5 Korean Medicine Clinical Trial Center, Korean Medicine Hospital, Kyung Hee University, Seoul, Republic of Korea
- 6 Acupuncture, Moxibustion & Meridian Research Group, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 7 Clinical Research Coordinating Team, Korea Institute of Oriental Medicine, Yuseong-daero 1672, Yuseong-gu, Daejeon, Republic of Korea
- 8 KM Data Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 9 Korean Convergence Medical Science, University of Science & Technology (UST), Daejeon, Republic of Korea
3. Results
3.1. Study Participants.
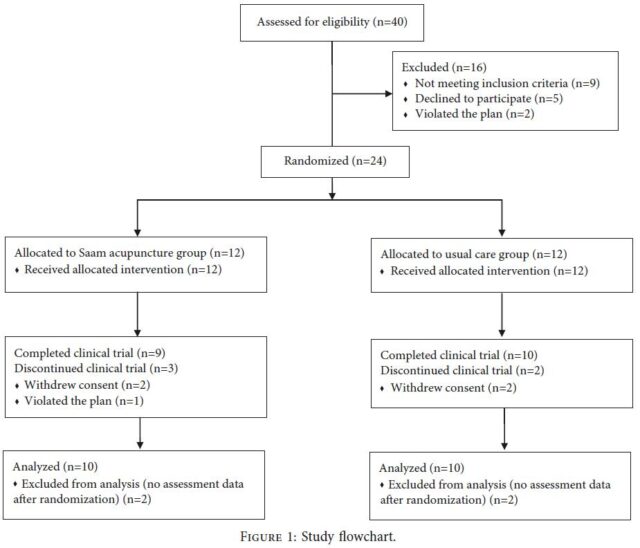
A total of 40 patients were assessed for eligibility. Among them, nine patients who did not meet the inclusion and exclusion criteria, five patients who declined to participate, and two patients who violated the protocol because they did not visit within 10 days of the screening visit were excluded. Twenty-four participants were randomly assigned 1 :1 to the Saam acupuncture plus usual care group or the usual care group (Figure 1).
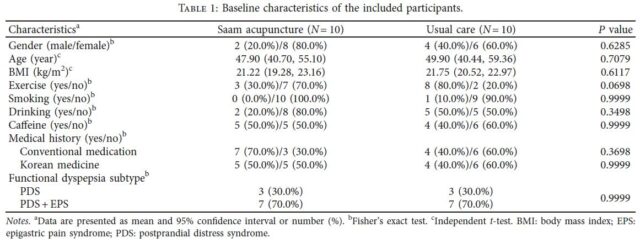
There were no significant differences in baseline demographic characteristics between the two groups, including sex, age, and medical history (Table1). There was no significant difference in eating habits between the two groups. The participants regularly ate at least twice a day and consumed stimulating foods (salty or spicy foods) or flour-based foods at most two to three times a week. Two participants in the acupuncture group and three participants in the usual care group took conventional medications such as acid suppressants and prokinetics during the study period.
 3.2. Feasibility.
3.2. Feasibility.
The recruitment rate was 60% (24/40) in this trial. A total of five participants (20.8%; three participants in the acupuncture group and two participants in the control group) dropped out after randomization. Among them, four participants (two participants in the acupuncture and control groups, resp.) withdrew their consent during the intervention period, and one participant in the acupuncture group was excluded due to him/her violating the study protocol by not attending the last follow-up visit (Week 12). There were no dropouts due to AEs. Therefore, the assessment of the final outcomes was completed for a total of 19 participants (nine participants in the acupuncture group and ten participants in the control group) at the last follow up visit (Week 12). .e completion rates in the acupuncture and control groups were 75% (9/12) and 83.3% (10/12), respectively (total, 79.2%). In the acupuncture group, the adherence rate was 83.3% (10/12). It took 21 months at one center to recruit all 24 participants (1.14 participants recruited per center per month), and there were no missing data collection values, except for those due to participants’ dropout.
3.3. Effectiveness.
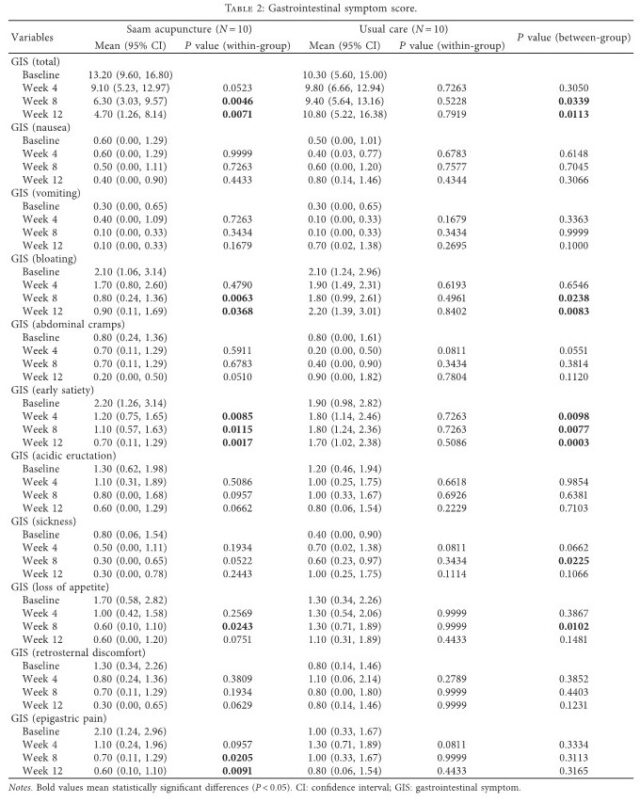
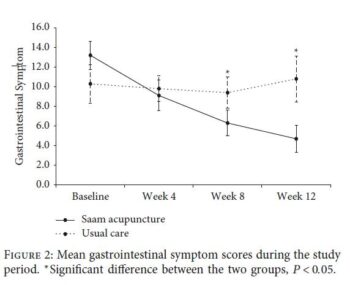 Although there was no significant difference between the two groups in total GIS scores at Week 4 (P = 0.3050), significant differences were found between the two groups at the follow-up assessments (Weeks 8 and 12; P = 0.0339 and 0.0113). After applying a repeated-measures analysis of variance, the GIS scores of the usual care group showed little change, while those of the acupuncture group continued to decrease after treatment (Figure 2).
Although there was no significant difference between the two groups in total GIS scores at Week 4 (P = 0.3050), significant differences were found between the two groups at the follow-up assessments (Weeks 8 and 12; P = 0.0339 and 0.0113). After applying a repeated-measures analysis of variance, the GIS scores of the usual care group showed little change, while those of the acupuncture group continued to decrease after treatment (Figure 2).
Among the 10 subitems of the GIS, the early satiety scores showed significant differences between the two groups during the treatment period, especially during Week 4 (P = 0.0098). In addition, there were significant differences between the two groups at Weeks 8 and 12 for the bloating scores (P = 0.0238 and 0.0083) and at Week 8 for the sickness (P = 0.0225) and loss of appetite scores (P = 0.0102). .e scores for epigastric pain, one of the main symptoms of FD, were significantly improved at Weeks 8 and 12 (P = 0.0205 and 0.0091) compared to the baseline scores only in the acupuncture group, although there was no significant difference between the two groups (Table 2).
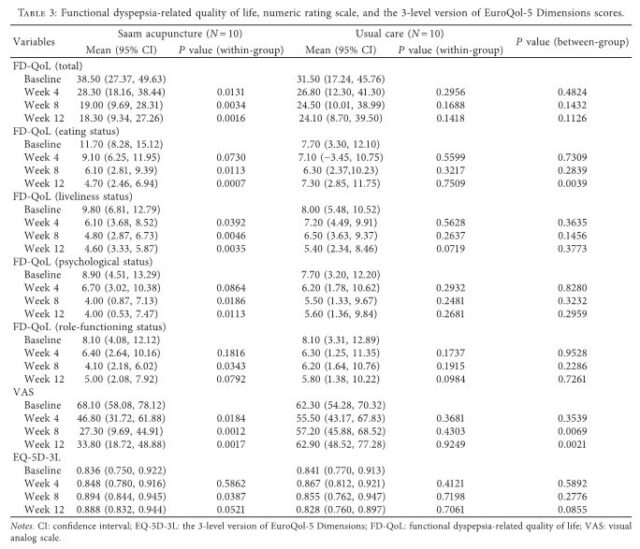
The FD-QoL scores were significantly improved compared to baseline only in the acupuncture group, but there was no significant difference between the two groups. However, among the FD-QoL subitems, there was a significant difference between the two groups for eating status at Week 12 (P = 0.0039). The scores for the VAS, which measured the intensity of dyspepsia symptoms, significantly improved during the treatment period in the acupuncture group, and there was a significant difference between the two groups at Weeks 8 and 12 (P = 0.0069 and 0.0021). The EQ-5D-3L scores were significantly improved compared to baseline at Week 8 (P = 0.0387) only in the acupuncture group, but there was no significant difference between the two groups (Table 3).
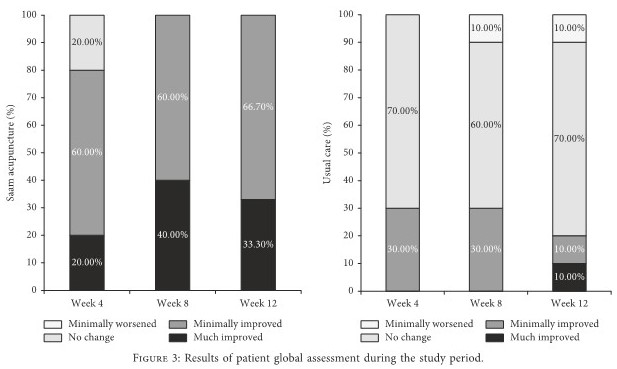
In the acupuncture group at Week 4, two participants (20%) described their condition as “much improved,” six (60%) as “minimally improved,” and two (20%) as “no change” compared to before treatment. In the usual care group, three (30%) described their condition as “minimally improved” and seven (70%) as “no change” compared to before treatment. At Week 8, four participants (40%) described their condition as “much improved” and six (60%) as “minimally improved” compared to before treatment in the acupuncture group, while three (30%) described their condition as “minimally improved,” six (60%) as “no change,” and one (10%) as “minimally worse” in the usual care group. At Week 12, three participants (33.3%) described their condition as “much improved” and six (66.7%) as “minimally improved” compared to before treatment in the acupuncture group, while one (10%) described their condition as “much improved,” one (10%) as “minimally improved,” seven (70%) as “no change,” and one (10%) as “minimally worse” in the usual care group. Although there was no significant difference in the PGA scores between the groups at Week 4 (P = 0.1025), there were statistically significant differences at Weeks 8 and 12 (P = 0.0026 and 0.0025) (Figure 3).
3.4. Safety.
During the clinical trial, one serious AE occurred in the usual care group due to hospitalization for a urinary stone. The symptoms were cured after extracorporeal shock wave lithotripsy, and it was judged to clearly not be related to acupuncture because it occurred in the usual care group.