- Mikyung Kim(1Department of Internal Medicine, College of Korean Medicine, Sangji University), Chang-ho Han(Department of Internal Medicine, College of Korean Medicine, Dongguk University)
- J Korean Med. 2021;42(4):75-101
3. Meta-analysis and evidence level
2) Effectiveness of cupping therapy as an add-on to conventional treatment
①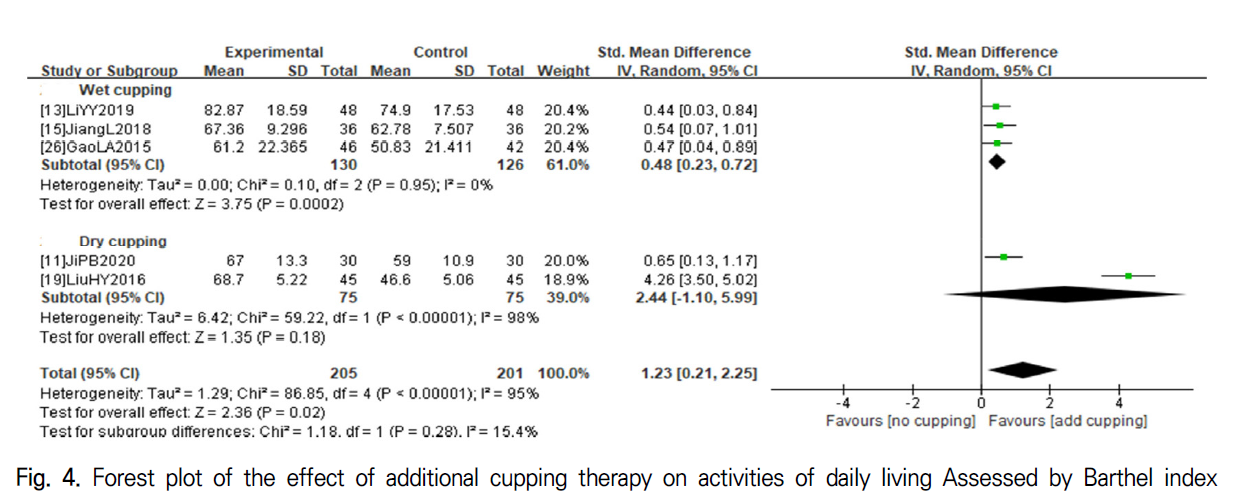 Activities of daily living (ADL) Five studies11,13,15,19,26) assessed the additive effect of cupping therapy using the Barthel index (BI) or modified Barthel index (MBI). Combining the data, the additional implementation of cupping therapy for patients who were receiving conventional treatment was significantly more advantageous than the noncupping condition (SMD 1.23, 95% CI 0.21 to 2.25, P=0.02) (Fig. 4), and the level of evidence supporting this result was low (Supplement 8). The subgroup analysis including only wet cupping studies13,15,26) showed similar results (SMD 0.48, 95% CI 0.23 to 0.72, P=0.0002) (Fig. 4). The heterogeneity detected in the whole synthesis (I2=95%) was resolved in the wet cupping subgroup analysis (I2=0%) (Fig. 4). However, when pooling the two studies involving only dry cupping11,19), the significant benefit of cupping therapy disappeared (SMD 2.44, 95% CI -1.10 to 5.99, P=0.18) (Fig. 4), and the level of evidence was also downgraded (Supplement 8).
Activities of daily living (ADL) Five studies11,13,15,19,26) assessed the additive effect of cupping therapy using the Barthel index (BI) or modified Barthel index (MBI). Combining the data, the additional implementation of cupping therapy for patients who were receiving conventional treatment was significantly more advantageous than the noncupping condition (SMD 1.23, 95% CI 0.21 to 2.25, P=0.02) (Fig. 4), and the level of evidence supporting this result was low (Supplement 8). The subgroup analysis including only wet cupping studies13,15,26) showed similar results (SMD 0.48, 95% CI 0.23 to 0.72, P=0.0002) (Fig. 4). The heterogeneity detected in the whole synthesis (I2=95%) was resolved in the wet cupping subgroup analysis (I2=0%) (Fig. 4). However, when pooling the two studies involving only dry cupping11,19), the significant benefit of cupping therapy disappeared (SMD 2.44, 95% CI -1.10 to 5.99, P=0.18) (Fig. 4), and the level of evidence was also downgraded (Supplement 8).
② Motor function
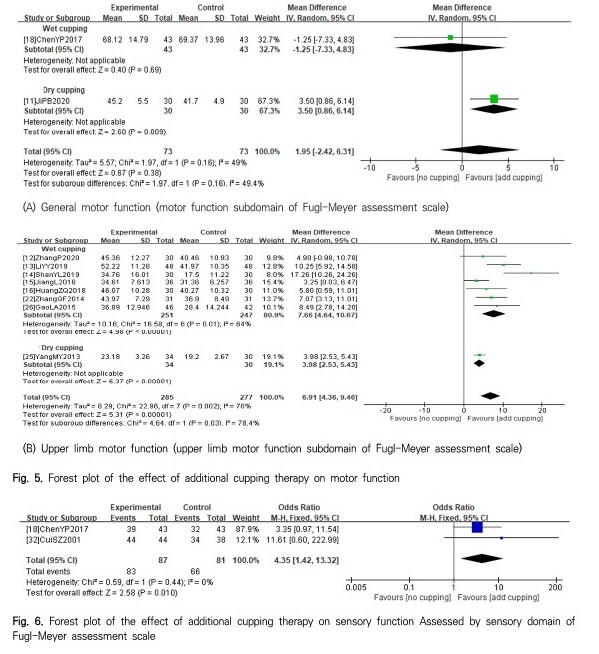 General motor function: Only wet cupping study18) and one dry cupping study11) evaluated the change in the motor function subdomain score on the FMA scale. Only the dry cupping study showed a significant benefit of cupping therapy (MD 3.50, 95% CI 0.86 to 6.14, P=0.009) (Fig. 5(A)). However, when combining the two studies, the additional benefits of cupping therapy were not confirmed (MD 1.95, 95% CI -2.42 to 6.31, P=0.38) (Fig. 5(A)), and the level of evidence was still very low (Supplement 8).
General motor function: Only wet cupping study18) and one dry cupping study11) evaluated the change in the motor function subdomain score on the FMA scale. Only the dry cupping study showed a significant benefit of cupping therapy (MD 3.50, 95% CI 0.86 to 6.14, P=0.009) (Fig. 5(A)). However, when combining the two studies, the additional benefits of cupping therapy were not confirmed (MD 1.95, 95% CI -2.42 to 6.31, P=0.38) (Fig. 5(A)), and the level of evidence was still very low (Supplement 8).- Upper limb motor function: Seven studies using wet cupping12-16,22,26) and one study using dry cupping25) reported changes in the upper limb motor function subdomain score of the FMA scale. All studies showed significantly beneficial effects of additive cupping therapy (Fig. 5(B)). Meta-analysis also showed positive results of cupping therapy (MD 6.91, 95% CI 4.36 to 9.46, P<0.00001) (Fig. 5(B)), which was supported by a moderate level of evidence (Supplement 6). The subgroup analysis including only wet cupping studies showed similar results (MD 7.66, 95% CI 4.64 to 10.67, P=0.01) (Fig. 5(B)) (Supplement 8).
- Sensory function: Two studies18,32) compared the response rates with and without additional wet cupping therapy in patients with sensory impairment after stroke. Meta-analysis of these studies showed that the benefit of wet cupping therapy was significant and the level of evidence supporting the result was low (OR 4.35, 95% CI 1.42 to 13.32, P=0.010) (Fig. 6) (Supplement 8).
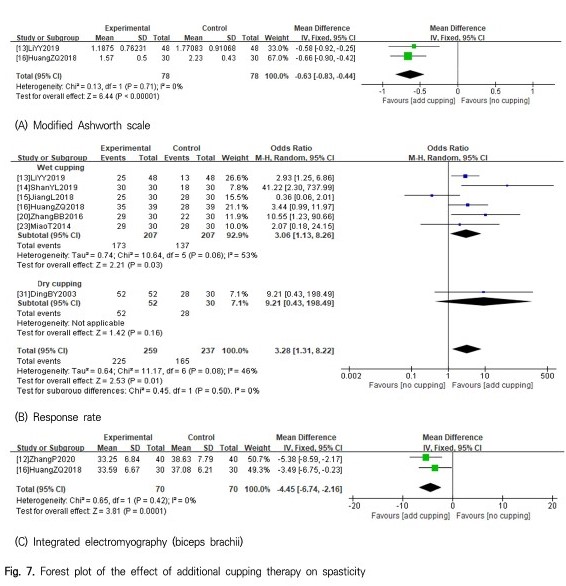 Spasticity: Two studies13,16) assessed the level of spasticity using the MAS before and after wet cupping therapy in patients with upper arm spasticity. The meta-analysis of these two studies showed that the additional effect of wet cupping was significant with a low level of evidence (MD -0.63, 95% CI -0.83 to -0.44, P<0.00001) (Fig. 7(A)) (Supplement 8). Seven studies13-15,20,23,31) investigated the proportion of participants who responded positively in terms of spasticity after cupping therapy. The meta -analysis of these studies showed the significant benefit of cupping therapy (OR 3.28, 95% CI 1.31 to 8.22, P=0.01) (Fig. 7(B)), and a moderate level of evidence supported this result (Supplement 8). The subgroup analysis of the wet cupping studies showed similar results (OR 3.06, 95% CI 1.13 to 8.26, P=0.03), whereas the dry cupping subgroup did not (OR 9.21, 95% CI 0.43 to 198.49, P=0.16) (Fig. 7(B)) (Supplement 8). Changes in biceps brachii muscle detected by integrated electromyography in patients with upper limb spasticity were also more favorable for wet cupping (MD -4.45, 95% CI -6.74 to -2.16, P=0.0001) (Fig. 7(C))12,16). However, the level of evidence supporting this benefit was very low (Supplement 8).
Spasticity: Two studies13,16) assessed the level of spasticity using the MAS before and after wet cupping therapy in patients with upper arm spasticity. The meta-analysis of these two studies showed that the additional effect of wet cupping was significant with a low level of evidence (MD -0.63, 95% CI -0.83 to -0.44, P<0.00001) (Fig. 7(A)) (Supplement 8). Seven studies13-15,20,23,31) investigated the proportion of participants who responded positively in terms of spasticity after cupping therapy. The meta -analysis of these studies showed the significant benefit of cupping therapy (OR 3.28, 95% CI 1.31 to 8.22, P=0.01) (Fig. 7(B)), and a moderate level of evidence supported this result (Supplement 8). The subgroup analysis of the wet cupping studies showed similar results (OR 3.06, 95% CI 1.13 to 8.26, P=0.03), whereas the dry cupping subgroup did not (OR 9.21, 95% CI 0.43 to 198.49, P=0.16) (Fig. 7(B)) (Supplement 8). Changes in biceps brachii muscle detected by integrated electromyography in patients with upper limb spasticity were also more favorable for wet cupping (MD -4.45, 95% CI -6.74 to -2.16, P=0.0001) (Fig. 7(C))12,16). However, the level of evidence supporting this benefit was very low (Supplement 8).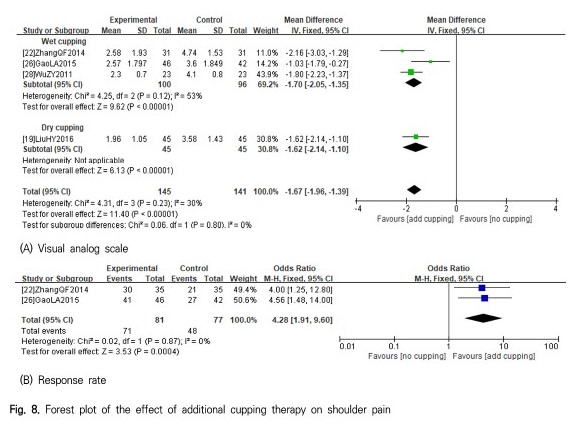 Shoulder pain: Four studies19,22,26,28) reported changes in shoulder pain measured by a VAS after additive cupping therapy for patients with hemiplegic shoulder pain. The meta-analysis of these studies showed that adjuvant cupping therapy had significant benefits in reducing VAS scores (MD -1.67, 95% CI -1.96 to -1.39, P<0.00001) (Fig. 8(A)), although the level of evidence supporting this effect was very low (Supplement 6). Similar results were reproduced in the subgroup analysis including only the wet cupping studies (MD -1.70, 95% CI -2.05 to -1.35) (Fig. 8(A)) (Supplement 8). Two studies22,26) investigated the proportion of hemiplegic shoulder pain patients who responded positively to wet cupping therapy. Combining these studies showed that additive wet cupping therapy had significant benefits in improving shoulder pain, although the level of evidence was very low (OR 4.28, 95% CI 1.91 to 9.60, P=0.0004) (Fig. 8(B)) (Supplement 8).
Shoulder pain: Four studies19,22,26,28) reported changes in shoulder pain measured by a VAS after additive cupping therapy for patients with hemiplegic shoulder pain. The meta-analysis of these studies showed that adjuvant cupping therapy had significant benefits in reducing VAS scores (MD -1.67, 95% CI -1.96 to -1.39, P<0.00001) (Fig. 8(A)), although the level of evidence supporting this effect was very low (Supplement 6). Similar results were reproduced in the subgroup analysis including only the wet cupping studies (MD -1.70, 95% CI -2.05 to -1.35) (Fig. 8(A)) (Supplement 8). Two studies22,26) investigated the proportion of hemiplegic shoulder pain patients who responded positively to wet cupping therapy. Combining these studies showed that additive wet cupping therapy had significant benefits in improving shoulder pain, although the level of evidence was very low (OR 4.28, 95% CI 1.91 to 9.60, P=0.0004) (Fig. 8(B)) (Supplement 8).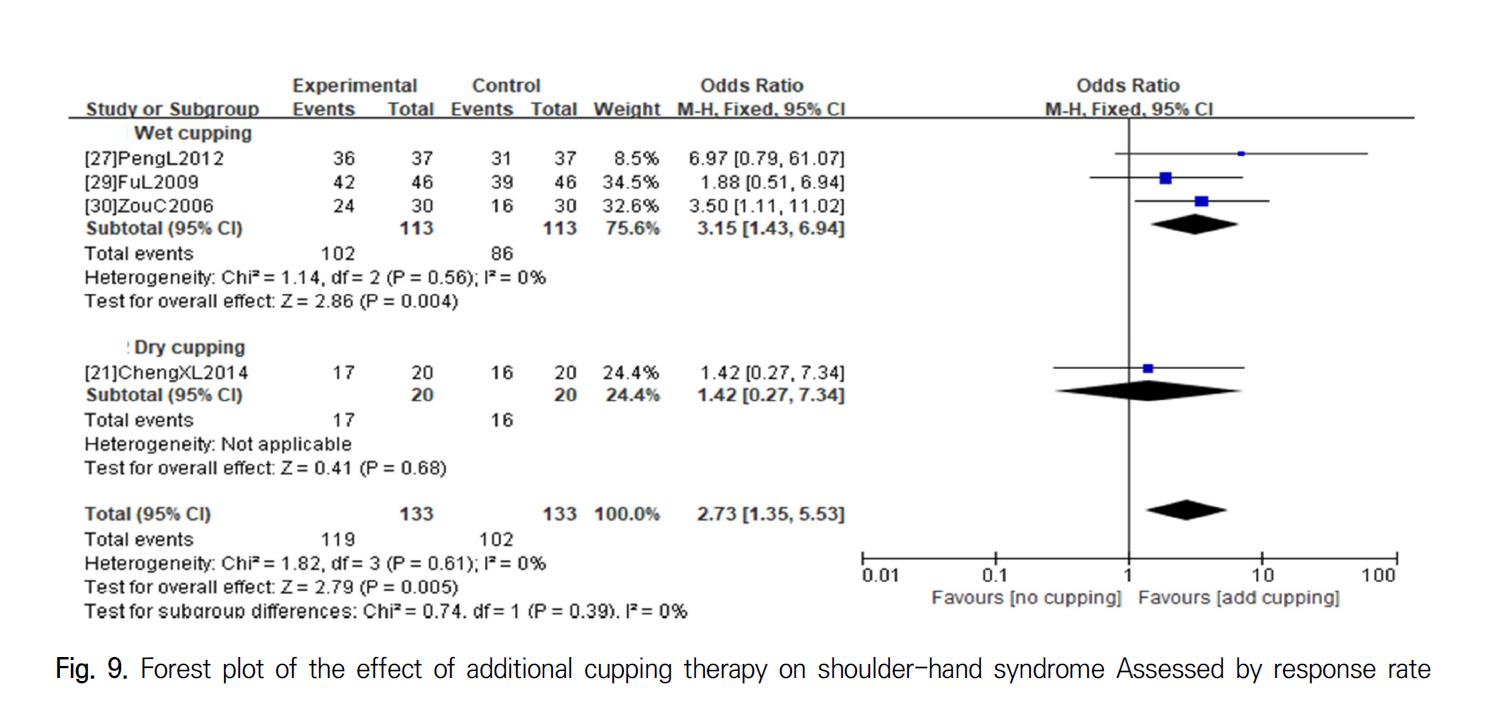 Shoulder-hand syndrome: Four studies21,27,29,30) assessed the response rates to cupping therapy for patients with poststroke shoulder-hand syndrome. The meta-analysis of these studies showed that cupping therapy had significant benefits in increasing the response rate in patients with poststroke shoulder-hand syndrome (OR 2.73, 95% CI 1.35 to 5.53, P=0.005) (Fig.9). The results of the subgroup analysis of studies involving only wet cupping therapy also reproduced similar results (OR 3.15, 95% CI 1.43 to 6.94, P=0.004) (Fig. 9). However, the level of evidence supporting these findings was very low in all cases (Supplement 8).
Shoulder-hand syndrome: Four studies21,27,29,30) assessed the response rates to cupping therapy for patients with poststroke shoulder-hand syndrome. The meta-analysis of these studies showed that cupping therapy had significant benefits in increasing the response rate in patients with poststroke shoulder-hand syndrome (OR 2.73, 95% CI 1.35 to 5.53, P=0.005) (Fig.9). The results of the subgroup analysis of studies involving only wet cupping therapy also reproduced similar results (OR 3.15, 95% CI 1.43 to 6.94, P=0.004) (Fig. 9). However, the level of evidence supporting these findings was very low in all cases (Supplement 8).- Safety: Five studies13,15,21,24,26) mentioned plans for collecting adverse events (AEs) during the study period. All of them were designed to compare the additional effectiveness of cupping therapy with the noncupping control. One24) of the five studies mentioned the AE collection plan in the Methods section of the article but did not provide any information on the safety profile in the Result section. Out of the 4 studies describing the intervention-related AEs in the Results section, one study21) was about dry cupping, and the others13,15,26) were about wet cupping. The dry cupping study21) reported that they did not identify any serious AEs in either cupping or noncupping groups. One of the wet cupping studies reported the occurrence of blistering with pain after cupping therapy, but did not disclose how many cases were identified26). Therefore, we could secure data available for meta-analysis from only two wet cupping studies13,15). One study provided wet cupping therapy every other day for 30 days to patients with upper arm spasticity and reported two cases of subcutaneous bleeding at the cupping site13). These AEs spontaneously disappeared after 1 week, and no AEs were identified in the control group13). Another study provided wet cupping therapy every other day for 3 months to patients with upper arm dysfunction and identified two cases of AEs, including either bleeding or pain15). Combining the AEs identified in these two studies, no significant difference was found in the occurrence of AEs between the additional cupping group and the noncupping control group (OR 6.33, 95% CI 0.74 to 53.99, P=0.09) (Fig. 10), and the level of evidence supporting this result was very low (Supplement 8).
References
- 11. Ji, P. B., Wu, Z. Q., Jia, D. P., Wang, L., & Shu, Y. Y. (2020). Clinical Study of Colored Silica Gel Can Combined with Exercise Therapy for Unilateral eglect After Stroke. Shanghai Journal of Acupuncture and Moxibustion, 39(8), 983-987. doi: 10.13460/ j.issn.1005-0957.2020.08.0983
- 12. Zhang, P., Chen, Y., Dai, W., & Nie, L. (2020). Observation on the effect of puncturing and cupping combined with rehabilitation training in the treatment of stroke patients with upper limb elbow flexion spasm and analysis of the effect of biceps integrated electromyography. China Rural Health, 12(20), 75.
- 13. Li, Y. (2019). Clinical Study of Blood – letting Puncture and Cupping Combined with Bobath Technique in the Treatment of Upper Limb Spasticity after Stroke. Chinese Journal of Ethnomedicine and Ethnopharmacy, 28(21), 84-86.
- 14. Shan, Y., Liu, J., Sun, L., Li, Q., & Wang, J. (2019). Therapeutic Observation of Collateral -pricking Cupping for Upper-limb Spasm in Patients with Cerebral Stroke. Shanghai Journal of Acupuncture and Moxibustion, 38(3), 270-274. doi: 10.13460/j.issn.1005-0957. 2019.03.0270.
- 15. Jiang, L. (2018). The Curative Effect of Acupuncture and Cupping Therapy on Upper Limb Dysfunction of Stroke Xinjiang Medical University [Master’s thesis].
- 16. Huang, Z., Zhao, N., Su, Z., Su, J., & Wu, Q. (2018). Effects of pricking and cupping combined with rehabilitation training on elbow flexion spasticity of upper limb after stroke and its IEMG value. Chinese Acupuncture & Moxibustion, 38(2), 119-124. doi: 10.13703/j.0255-2930.2018.02.002.
- 17. Chen, J., Lin, S. (2017). The clinical effect of pricking and cupping combined with rehabilitation training in the treatment of stroke patients with upper limb elbow flexion spasm. Chinese Journal of Medical Device, 30(15), 121-122.
- 18. Chen, Y. P. (2017). Clinical Research on Hemidysesthesia After Stroke Treated by Acupuncture combined with Collateral-Needling Cupping. Henan Traditional Chinese Medicine, 37(1), 87-89. doi: 10.16367/j.issn.1003-5028.
2017.01.0029. - 19. Liu, H., Liu, T., & Wang, Z. (2016). Effect of acupoint injection combined with cupping treatment on the daily life ability of patients with shoulder pain after stroke. Chinese Community Doctors, 32(27), 169-170. doi: 10.3969/j.issn.1007-614x.2016.27.108.
- 20. Zhang, B. (2016). The Clinical Observation of Body Spasm After Stroke Applying The Therapy of Combination Acupucture With Pricking and Cupping. Shandong University of Traditional Chinese Medicine [Master’s thesis].
- 21. Cheng, X., Cheng, C. (2014). Cupping combined Conventional Symptomatic Treatment and Rehabilitation Training after Stroke Shoulder – hand Syndrome Randomized Parallel Group Study. Journal of Practical Traditional Chinese Internal Medicine, 28(11), 27-29. doi: 10.13729/j.issn.1671-7813.2014.11.12.
- 22. Zhang, Q., Wei, Z., Cui, Y. (2014), Bloodletting and cupping combined with exercise therapy to treat 31 cases of stroke and hemiplegia and shoulder pain.. Hebei Journal of Traditional Chinese Medicine, 36(4), 568-569.
- 23. Miao, T. (2014). MOTOmed intelligent exercise system combined with blood pricking and cupping for treatment of increased muscle tone of lower limbs in stroke patients. Practical Journal of Medicine and Pharmacy, 31(3), 214-215. doi: 10.14172/j.cnki.issn1671 -4008.2014.03.007.
- 24. Huang, Z. (2014). Effect of Pricking Blood with Cupping Therapy Combined with Rehabilitation Training on the Spasticity of the Upper Limb in Patients with Stroke. Fujian University of Traditional Chinese Medicine [Master’s thesis].
- 25. Yang, M. (2013). Rehabilitation training combined with cupping to treat 64 cases of shoulder pain after stroke. Forum on Traditional Chinese Medicine, 28(6), 26-27.
- 26. Gao, L., Chu, J., & Bao, Y. (2012). Observation on the effect of blood puncturing and cupping combined with rehabilitation on hemiplegic shoulder pain and upper limb motor function improvement after stroke. Zhejiang Journal of Traditional Chinese Medicine, 47(11), 821-823.