A Patient With Long COVID-19 Symptoms
By David Lee, L.Ac.
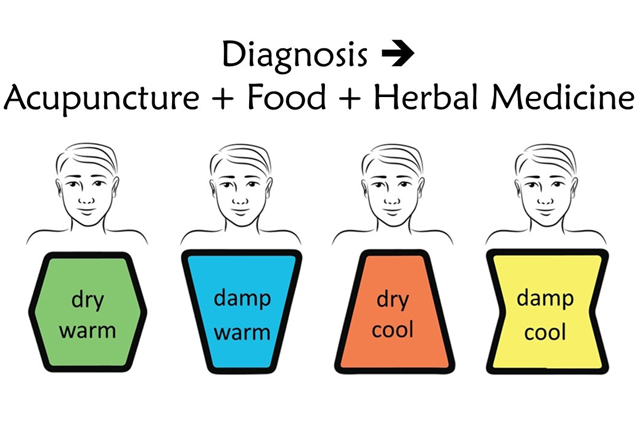
Constitutional acupuncture, dietary adjustments, and herbal medicine offer viable pathways to recover from long COVID symptoms. Here, we share the journey of Mary L., a schoolteacher and graduate student who battled persistent symptoms for 14 months.
Mary’s struggle encompassed mental and physical challenges, making it daunting to fulfill her daily responsibilities as both a teacher and a student pursuing a master’s degree. Lingering symptoms included mind and body fatigue, persistent pain from her left hip down to her foot, generalized aches, headaches, shortness of breath, loss of appetite, and a metallic taste. Fogginess was exacerbated by simple sugars.
Teaching and academic pursuits were difficult, given the demanding requirements of reading, writing, and meetings. Persistent headaches were attributed to seasonal hay fever and were associated with the menstrual cycle. Effective self-treatment measures included engaging in gentle exercise, utilizing infrared heat therapy, and ensuring adequate Vitamin D intake.
Mary’s first acupuncture points were right-side Yang Horary points in Metal-Order of LI1 (Metal), UB66 (Water), GB41 (Wood), SI5 (Fire), and ST36 (Earth). This treatment aided in restoring her mental clarity to its pre-COVID state, allowing her to confidently teach the next day in front of her class. Following the second treatment, she experienced a return to normalcy in both mind and body. Notably, even after engaging in exercise, her fatigue did not worsen, and the usual intensity of her period headache was below average. This positive response provided her with the first glimpse of the possibility of a substantial recovery, instilling a sense of encouragement.
However, following her fourth visit, she had to be admitted to the hospital due to a resurgence of symptoms after engaging in moderate exercise twice for 40 minutes. She received an intravenous infusion of glutathione, vitamin C, and vitamin B complex to aid recovery.
From the 7th to the 10th visit, conducted once a week, she received additional Fire points SI5 (Fire), UB60 (Fire), and GB38 (Fire), which proved to be even more beneficial. The diagnosis revealed a combination of Lesser Yin (Excess Water, Deficient Earth, and Deficient Fire) and Greater Yang (Excess Metal and Deficient Wood) in Tetrasoma acupuncture.
In Sasang Korean medicine, she was a Soeumin constitution, while Ayurvedic medicine identified her as Vata. Unani medicine from the Middle East and Africa categorized her as Phlegmatic. Additionally, she was identified as having an Affiliation in the Need Theory of America, a Steady profile in the Social Styles of America, and fell under the ENFJ, INFJ, ENTJ, and INTJ categories in the Myers-Briggs system. These diverse diagnostic perspectives were contributed by the global medical community.
Subsequently, acupuncture treatments were adjusted to once every two weeks due to the financial constraints of being a student, and she expressed contentment with the progress. Over time, there was a gradual and consistent enhancement in her symptoms’ intensity, frequency, and duration, leading to more days of feeling normal.
In the third month, she was introduced to an herbal medicine to her regimen. Despite consuming only one-third of the average dosage, there was a progressive and steady improvement in her condition.
Mary minimized the intake of constitutionally harmful foods such as nuts, pork, shellfish, celery, and cucumber.
During the initial three months, she was prescribed Gui Zhi Ban Xia Sheng Jiang Tang due to abdominal bloating after meals, epigastric fullness, and general under-the-weather symptoms. Thereafter, Xiang Sha Yang Wei Tang, Shi Quan Da Bu Tang, and a combination including Korean red ginseng were prescribed.
Her progress was gradual and consistently improved month by month. This positive development enabled her to manage the demands of graduate studies and work, ultimately earning her a full scholarship at the University of Kentucky. At the end of 18 months, her overall relief was assessed at 90%.
Although the loss of smell remained unaffected, I successfully restored the sense of smell for another individual with a similar constitution using a gall bladder/kidney formula for stones, consisting of San Leng, E Zhu, Hai Jin Sha, Dan Shen, Jin Qian Cao, and Shi Wei.
She continues to adhere to a maintenance dosage of herbal medicine, ensuring continuous support for her health and well-being. This holistic approach improves mental and physical functioning, enriching her life with added years.